Evidence and Practice

How do I recognise and respond to signs of burnout in myself and colleagues in the ED?
A strategic solution to preventing the harm associated with ambulance handover delays
Improving suicide risk screening in the emergency department
Clinical
A strategic solution to preventing the harm associated with ambulance handover delays
Why you should read this article: • To recognise that overcrowded emergency departments result in ambulance handover delays causing avoidable harm to patients awaiting assessment • To identify how forward planning and anticipatory escalation processes can reduce the potential for patients to experience avoidable harm • To learn how a strategic quality improvement project improved patient safety and the working lives of front-line healthcare professionals Ambulance handover delays arise when emergency departments become overcrowded as patients waiting prolonged periods for admission occupy clinical cubicles designed to facilitate the assessment and treatment of emergency arrivals. In response, many organisations become reliant on temporarily lodging acutely unwell patients awaiting admission in undesignated areas for care such as corridors, to provide additional space. This results in a significant risk of avoidable harm, indignity and psychological trauma for patients and has a negative effect on the well-being of healthcare professionals, since unacceptable standards of care become normalised. A two-phase strategic quality improvement project was implemented at the authors’ acute trust. Ambulance handover data from between 2 November 2020 and 26 July 2021 provided a benchmark for the project. The first phase was implemented between 2 November 2021 and 26 July 2022 and aimed to reduce 60-minute ambulance handover delays. The second phase was implemented between 2 November 2022 and 26 July 2023 and aimed to eradicate 60-minute ambulance handover delays and improve overall performance. Phase one resulted in a 32% reduction in 60-minute ambulance handover delays. Phase two resulted in a 97% reduction in 60-minute ambulance handover delays. Over the course of the project there was a 24% increase in handovers completed within 15 minutes. This project demonstrates how strategic planning and collaboration between healthcare teams can reduce the potential for avoidable patient harm, while simultaneously promoting workforce well-being and retention.
Improving suicide risk screening in the emergency department
Learn about the use of the Columbia-Suicide Severity Risk Scale
Developing a major trauma course and coaching programme for ward nurses
A bespoke course is helping to increase nurses’ competence when caring for patients with complex trauma
Reducing the burden on ambulance services and EDs: a mental health initiative
How mental health professionals worked with 999 call centre clinical support in Wales
Nitrous oxide tank cold burn to forearm: case study and discussion of the literature
N2O burn presentations are increasingly common in EDs, pointing to need for more formal care guidelines
Using body-worn cameras in emergency departments: a pilot project
A rise in violence at one trust prompted the introduction of body-worn cameras
CPD articles
Blunt mechanism chest wall injury: initial patient assessment and acute care priorities
A prognostic model predicting complications helps nurses to asses risk and level of care required
Maintaining a safe environment in emergency department waiting rooms
How nurses can manage patients' expectations in a busy and unpredictable environment
‘Corridor care’ in the ED: managing patient care in non-clinical areas safely
The unique challenges of having to care for patients in non-clinical areas
Overcoming the barriers to optimal end of life care in the emergency department
Nurses working in EDs can help ensure that the care needs of dying patients and their families are addressed
Managing infection prevention and control in emergency care
Overview of epidemiological perspectives including the nurse’s role in antibiotic stewardship
Recognition and management of patients with frailty in the emergency department
Familiarise yourself with frailty screening tools often used in emergency care settings
How to
How to break bad news
A step-by-step framework nurses can use when having challenging conversations
How to improve patient care by learning from mistakes
Mistakes made in healthcare settings and the challenges to staff that arise from them can harm service users, consume time and money, and often receive bad publicity. However, by learning from these mistakes and meeting these challenges, practitioners can improve the quality of the care they provide. This article explores what is meant by mistakes and challenges in the context of health care. It suggests that front line managers are best placed to prevent and learn from mistakes, and thereby improve care for patients.
Practice question
How do I recognise and respond to signs of burnout in myself and colleagues in the ED?
Advice on recognising burnout in yourself and others, and where to find support
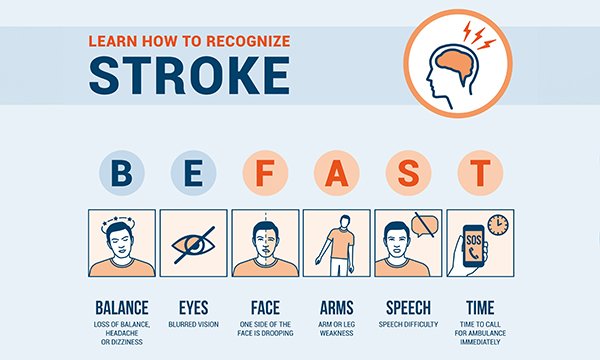
How can I identify the signs of a posterior stroke?
It can be difficult to recognise the symptoms, but the BEFAST acronym can help
How do I talk sensitively to people who are living with obesity about weight and health?
Even short conversations about weight can help patients, but avoid suggesting blame
How can I improve my patient triage skills in the emergency department?
Decision-making, patient assessment and triage algorithms are important skills to develop
What should an ED team debrief involve and how do I lead one?
Emergency departments are high-pressured and debriefings can help sustain a healthy workplace
How can you identify and manage people presenting with delirium in the ED?
The condition can develop quickly and result in increased risk of dementia and mortality